Efecto de la aplicación de anticoagulante sistémico (ácido acetilsalicílico) en la osteointegración de implantes en tibias de rata en trasplante óseo alogénico
Resumen
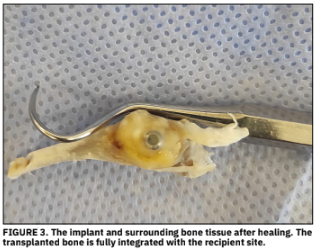
Es t e es tudio tuv o c omo objetiv o in v es tig ar el ef ect o de la administración sistémica de ácido acetilsalicílico, utilizado en el tratamiento de la enfermedad arterial coronaria, sobre el nivel de osteointegración de implantes de titanio en el hueso trasplantado en el tratamiento de defectos óseos creados en tibias de rata mediante trasplante óseo alogénico. En este estudio se utilizaron cuarenta y dos ratas Sprague Dawley hembras, de entre 6 y 12 meses de edad. El peso promedio de las ratas fue de entre 270 y 300 gramos. Para evitar daños a los animales durante el experimento, la temperatura se controló constantemente y se implementó un ciclo de 12 horas de luz/12 horas de oscuridad. Esto indica diferencias significativas entre los grupos. En general, entre los grupos sin aloinjerto, el valor medio de contacto hueso-implante fue 6,31 (Mediana: 6,30) en el grupo control, mientras que el valor fue 6,40 (6,20) en el grupo de ácido acetilsalicílico dosis 1. No se encontraron diferencias significativas entre estos dos grupos. En el grupo de ácido acetilsalicílico dosis 2, se obtuvo el valor de 6,51 (6,80), mientras que, se observó un aumento en comparación con los grupos control y de ácido acetilsalicílico dosis 1, pero no se obtuvieron diferencias significativas. En este estudio, los resultados demostraron los efectos beneficiosos del ácido acetilsalicílico. Se lograron mayores tasas de fusión hueso-implante en los grupos tratados con ácido acetilsalicílico. Se concluye que el uso de ácido acetilsalicílico puede ser beneficioso en casos que requieren aumento óseo.
Descargas
Citas
Elani HW, Starr JR, Da Silva JD, Gallucci GO. Trends in Dental Implant Use in the U.S., 1999-2016, and Projections to 2026. J. Dent. Res. [Internet]. 2018; 97(13):1424-1430. doi: https://doi.org/gd2rfw
Kapil N, Datta YH, Alakbarova N, Bershad E, Selim M, Liebeskind DS, Bachour O, Rao GHR, Divani AA. Antiplatelet and Anticoagulant Therapies for Prevention of Ischemic Stroke. Clin. Appl. Thromb. Hemost. [Internet]. 2016; 23(4):301-318. doi: https://doi.org/f9trh9
Mega JL, Simon T. Pharmacology of antithrombotic drugs: an assessment of oral antiplatelet and anticoagulant treatments. Lancet. [Internet]. 2015; 386(9990):281-291. doi: https://doi.org/f3hdfs
Raimondi P, Hylek EM, Aronis KN. Reversal Agents for Oral Antiplatelet and Anticoagulant Treatment During Bleeding Events: Current Strategies. Curr. Pharm. Des. [Internet]. 2017; 23(9):1406-1423. doi: https://doi.org/f97jn4
de Souza-Rendohl E, Miziara LNB, Pimentel AC, Sendyk WR, Santiago-Junior JF, Marão HF. The influence of acetylsalicylic acid on bone regeneration: systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. [Internet]. 2021; 59(10):E1-E16. doi: https://doi.org/gpdhxd
Miguita L, Mantesso A, Pannuti CM, Deboni MCZ. Can stem cells enhance bone formation in the human edentulous alveolar ridge? A systematic review and meta-analysis. Cell. Tissue Bank. [Internet]. 2017; 18(2):217-228. doi: https://doi.org/qqcc
Li B, Xu J, Hall AJ, Haupt K, Tse-Sum-Bui B. Watercompatible silica sol-gel molecularly imprinted polymer as a potential delivery system for the controlled release of salicylic acid. J. Mol. Recognit. [Internet]. 2014; 27(9):559-565. doi: https://doi.org/f59386
Tang Y, Singh J. Controlled delivery of aspirin: effect of aspirin on polymer degradation and in vitro release from PLGA based phase sensitive systems. Int. J. Pharm. [Internet]. 2008; 357(1-2):119-125. doi: https://doi.org/b2p9g4
Liu Y, Chen C, Liu S, Liu D, Xu X, Chen X, Shi S. Acetylsalicylic acid treatment improves differentiation and immunomodulation of SHED. J. Dent. Res. [Internet]. 2015; 94(1):209-218. doi: https://doi.org/f6thpf
Fijalkowski L, Skubiszewska M, Grzesk G, Koech FK, Nowaczyk A. Acetylsalicylic Acid-Primus Inter Pares in Pharmacology. Molecules. [Internet]. 2022; 27(23):8412. doi: https://doi.org/qqcd
Balakumaran A, Mishra PJ, Pawelczyk E, Yoshizawa S, Sworder BJ, Cherman N, Kuznetsov SA, Bianco P, Giri N, Savage SA, Merlino G, Dumitriu B, Dunbar CE, Young NS, Alter BP, Robey PG. Bone marrow skeletal stem/progenitor cell defects in dyskeratosis congenita and telomere biology disorders. Blood. [Internet]. 2015; 125(5):793802. doi: https://doi.org/gr8ccp
Chen C, Akiyama K, Yamaza T, You YO, Xu X, Li B, Zhao Y, Shi S. Telomerase governs immunomodulatory properties of mesenchymal stem cells by regulating FAS ligand expression. EMBO Mol. Med. [Internet]. 2014; 6(3):322334. doi: https://doi.org/f2qg4g
Cao Y, Xiong J, Mei S, Wang F, Zhao Z, Wang S, Liu Y. Aspirin promotes bone marrow mesenchymal stem cellbased calvarial bone regeneration in mini swine. Stem. Cell Res. Ther. [Internet]. 2015; 6:210. doi: https://doi.org/gpdh4k
Fang X, Lei L, Jiang T, Chen Y, Kang Y. Injectable thermosensitive alginate/ß-tricalcium phosphate/aspirin hydrogels for bone augmentation. J. Biomed. Mater. Res. B Appl. Biomater. [Internet]. 2018; 106(5):1739-1751. doi: https://doi.org/gpdh46
Shi S, Yamaza T, Akiyama K. Is aspirin treatment an appropriate intervention to osteoporosis? Fut. Rheumatol. [Internet]. 2008; 3(6):499-502. doi: https://doi.org/d6msmf
Tang J, Xiong J, Wu T, Tang Z, Ding G, Zhang C, Wang S, Liu Y. Aspirin treatment improved mesenchymal stem cell immunomodulatory properties via the 15d-PGJ2/PPAR./TGF-ß1 pathway. Stem. Cells Dev. [Internet]. 2014; 23(17):2093-2103. doi: https://doi.org/f6d9wv
Tonetti MS, Cortellini P, Lang NP, Suvan JE, Adriaens P, Dubravec D, Fonzar A, Fourmousis I, Rasperini G, Rossi R, Silvestri M, Topoll H, Wallkamm B, Zybutz M. Clinical outcomes following treatment of human intrabony defects with GTR/bone replacement material or access flap alone. A multicenter randomized controlled clinical trial. J. Clin. Periodontol. [Internet]. 2004; 31(9):770-776. doi: https://doi.org/cmdgj7
Wang W, Yeung KWK. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. [Internet]. 2017; 2(4):224-247. doi: https://doi.org/gdg7mk
Kao RT, Nares S, Reynolds MA. Periodontal regeneration - intrabony defects: a systematic review from the AAP Regeneration Workshop. J. Periodontol. [Internet]. 2015; 86(2S):77-104. doi: https://doi.org/gn6jwk
Bowers GM, Chadroff B, Carnevale R, Mellonig J, Corio R, Emerson J, Stevens M, Romberg E. Histologic evaluation of new attachment apparatus formation in humans. Part I. J. Periodontol. [Internet]. 1989; 60(12):664-674. doi: https://doi.org/qqcf
Coimbra LS, Steffens JP, Rossa C Jr, Graves DT, Spolidorio LC. Clopidogrel enhances periodontal repair in rats through decreased inflammation. J. Clin. Periodontol. [Internet]. 2014; 41(3):295-302. doi: https://doi.org/f5qt6n
Xiaoxin Z, Zhang J, Shi B. Mesoporous bioglass/silk fibroin scaffolds as a drug delivery system: Fabrication, drug loading and release in vitro and repair calvarial defects in vivo. J. Wuhan Univ. Technol. Mater. Sci. [Internet]. 2014; 29:401-406. doi: https://doi.org/qqcm
Jiang W, Zhan Y, Zhang Y, Sun D, Zhang G, Wang Z, Chen L, Sun J. Synergistic large segmental bone repair by 3D printed bionic scaffolds and engineered ADSC nanovesicles: Towards an optimized regenerative microenvironment. Biomaterials. [Internet]. 2024; 308:122566. doi: https://doi.org/gtrngf
Lillis T, Veis A, Sakellaridis N, Tsirlis A, Dailiana Z. Effect of clopidogrel in bone healing-experimental study in rabbits. World J. Orthop. [Internet]. 2019; 10(12):434-445. doi: https://doi.org/qqcg
Camacho-Alonso F, Martínez-Ortiz C, Plazas-Buendía L, Mercado-Díaz AM, Vilaplana-Vivo C, Navarro JA, Buendía AJ, Merino JJ, Martínez-Beneyto Y. Bone union formation in the rat mandibular symphysis using hydroxyapatite with or without simvastatin: effects on healthy, diabetic, and osteoporotic rats. Clin. Oral Investig. [Internet]. 2020; 24(4):1479-1491. doi: https://doi.org/qqch
Faruq O, Sayed S, Kim B, Im SB, Lee BT. A biphasic calcium phosphate ceramic scaffold loaded with oxidized cellulose nanofiber-gelatin hydrogel with immobilized simvastatin drug for osteogenic differentiation. J. Biomed. Mater. Res. B Appl. Biomater. [Internet]. 2020; 108(4):1229-1238. doi: https://doi.org/qqcj
D'Mello S, Atluri K, Geary SM, Hong L, Elangovan S, Salem AK. Bone Regeneration Using Gene-Activated Matrices. AAPS J. [Internet]. 2017;19(1):43-53. doi: https://doi.org/gn3jwm
Vlajic Tovilovic T, Petrovic S, Lazarevic M, Pavic A, Plackic N, Milovanovic A, Miloševic M, Miletic V, Veljovic D, Radunovic M. Effect of Acetylsalicylic Acid on Biological Properties of Novel Cement Based on Calcium Phosphate Doped with Ions of Strontium, Copper, and Zinc. Int. J. Mol. Sci. [Internet]. 2024;25(14):7940. doi: https://doi.org/qqck
Wada K, Yu W, Elazizi M, Barakat S, Ouimet MA, Rosario-Meléndez R, Fiorellini JP, Graves DT, Uhrich KE. Locally delivered salicylic acid from a poly(anhydride-ester): impact on diabetic bone regeneration. J. Control. Release. [Internet]. 2013; 171(1):33-37. doi: https://doi.org/f48swk
Coimbra LS, Steffens JP, Alsadun S, Albiero ML, Rossa C Jr, Pignolo RJ, Spolidorio LC, Graves DT. Clopidogrel Enhances Mesenchymal Stem Cell Proliferation Following Periodontitis. J. Dent. Res. [Internet]. 2015; 94(12):16911697. doi: https://doi.org/f7zxk2
Li X, Liu X, Ni S, Liu Y, Sun H, Lin Q. Enhanced osteogenic healing process of rat tooth sockets using a novel simvastatin-loaded injectable microspherehydrogel system. J. Craniomaxillofac. Surg. [Internet]. 2019;47(7):1147-1154. doi: https://doi.org/gpnbsx
Subramanian S, Mitchell A, Yu W, Snyder S, Uhrich K, O'Connor JP. Salicylic Acid-Based Polymers for Guided Bone Regeneration Using Bone Morphogenetic Protein-2. Tissue Eng. Part A. [Internet]. 2015; 21(13-14):20132024. doi: https://doi.org/f7xd7m
Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS, Koval KJ. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J. Orthop. Trauma. [Internet]. 2019; 33(4):203-213. doi: https://doi.org/gmtzbb
Hadzik J, Blaszczyszyn A, Gedrange T, Dominiak M. Soft-Tissue Augmentation around Dental Implants with a Connective Tissue Graft (CTG) and Xenogeneic Collagen Matrix (CMX)-5-Year Follow-Up. J. Clin. Med. [Internet]. 2023; 12(3):924. doi: https://doi.org/g7kzdg
Heinemann F, Mundt T, Biffar R, Gedrange T, Goetz W. A 3-year clinical and radiographic study of implants placed simultaneously with maxillary sinus floor augmentations using a new nanocrystalline hydroxyapatite. J. Physiol. Pharmacol. [Internet]. 2009 [cited 25 Aug 2025]; 60(8):91-97. Available in: https://goo.su/rKUZ
Hadzik J, Kubasiewicz-Ross P, Nawrot-Hadzik I, Gedrange T, Pitulaj A, Dominiak M. Short (6 mm) and Regular Dental Implants in the Posterior Maxilla-7-Years Follow-up Study. J. Clin. Med. [Internet]. 2021; 10(5):940. doi: https://doi.org/g774bg
Zhao R, Yang R, Cooper PR, Khurshid Z, Shavandi A, Ratnayake J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules. [Internet]. 2021; 26(10):3007. doi: https://doi.org/gsmsrh
Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. [Internet]. 2012; 8(4):114-124. doi: https://doi.org/g9dx3m
Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: an update. Injury. [Internet]. 2005; 36(3):20-27. doi: https://doi.org/cttm9f
Ciszynski M, Dominiak S, Dominiak M, Gedrange T, Hadzik J. Allogenic Bone Graft in Dentistry: A Review of Current Trends and Developments. Int. J. Mol. Sci. [Internet]. 2023; 24(23):16598. doi: https://doi.org/qqcn
Dias RR, Sehn FP, de Santana-Santos T, Silva ER, Chaushu G, Xavier SP. Corticocancellous fresh-frozen allograft bone blocks for augmenting atrophied posterior mandibles in humans. Clin. Oral Implants Res. [Internet]. 2016; 27(1):39-46. doi: https://doi.org/f772xk
Yamaza T, Miura Y, Bi Y, Liu Y, Akiyama K, Sonoyama W, Patel V, Gutkind S, Young M, Gronthos S, Le A, Wang CY, Chen W, Shi S. Pharmacologic stem cell based intervention as a new approach to osteoporosis treatment in rodents. PLoS One. [Internet]. 2008; 3(7):e2615. doi: https://doi.org/c4gxsz
Liu Y, Wang L, Kikuiri T, Akiyama K, Chen C, Xu X, Yang R, Chen W, Wang S, Shi S. Mesenchymal stem cellbased tissue regeneration is governed by recipient T lymphocytes via IFN-. and TNF-a. Nat. Med. [Internet]. 2011; 17(12):1594-1601. doi: https://doi.org/brr7bb
Zhang Y, Xiong Y, Chen X, Chen C, Zhu Z, Li L. Therapeutic effect of bone marrow mesenchymal stem cells pretreated with acetylsalicylic acid on experimental periodontitis in rats. Int. Immunopharmacol. [Internet]. 2018; 54:320328. doi: https://doi.org/gczdr5
Li H, Zhang Y, Du S, Shen J, Liu X, Jing J. "Remodeling the intestinal immune microenvironment": immune regulation and tissue regeneration by mesenchymal stem/stromal cells in the repair microenvironment of inflammatory bowel disease. Front. Immunol. [Internet]. 2025; 16:1543702. doi: https://doi.org/qqcp
Zhang Y, Dou X, Zhang L, Wang H, Zhang T, Bai R, Sun Q, Wang X, Yu T, Wu D, Han B, Deng X. Facile fabrication of a biocompatible composite gel with sustained release of aspirin for bone regeneration. Bioact. Mater. [Internet]. 2022; 11:130-139. doi: https://doi.org/gn4nxh